
People wait to have a chest X-ray as part of an active case-finding campaign for tuberculosis. This event took place in a rural district of An Giang province, Viet Nam. Mobile X-ray technology can be used in very rural areas. Photo credit: Hien Vu/FHI 360
Tuberculosis (TB) is once again the world’s most deadly infectious disease, silently retaking the top spot from COVID-19 sometime in mid-2022. TB sickens more than 10 million people each year and kills about 1.6 million, according to the World Health Organization (WHO).
Ending TB feels frustratingly out of reach, despite having excellent diagnostics to detect the disease and effective medicines to cure it. Just last year, the world did not meet the United Nations’ 2022 TB treatment and prevention targets, which were set in 2018.
As programs rush to catch up after the COVID-19 pandemic, now is the time to optimize existing tools to improve access to screening and accelerate case finding. Through FHI 360’s U.S. Agency for International Develop (USAID) Support to End Tuberculosis project in Viet Nam, we have honed the Double X strategy, a TB case-finding strategy that is accurate, comprehensive and adaptable.
Building a strong foundation for case finding with the latest technologies
Viet Nam has had a high burden of TB for decades, and it still does today. Since 2020, FHI 360 has worked with the country’s National Tuberculosis Program to find more people with TB, guarantee access to molecular WHO-recommended rapid diagnostics and incorporate preventive treatment into the TB program for high-risk individuals.
We are doing this through the Double X strategy, which uses chest X-ray to find people who have signs of pulmonary TB and triage them for more expensive GeneXpert molecular testing to confirm the diagnosis. Chest X-ray is highly sensitive and GeneXpert is highly specific, creating a high-performance strategy to diagnose TB.
This foundational strategy is flexible enough that no one with TB is missed, no matter where they go to seek care. We use Double X at community mobile health screening events and at health care facilities. It can also be done in very remote areas by bringing in portable X-ray technology and point-of-care molecular diagnostics. During COVID-19, our project designed adaptations to reach out to communities and refer them to Double X testing locations, and some of these adaptations are still being used today. We can use criteria to tailor the strategy to various risk groups for TB in a variety of settings.
Improving TB diagnosis with artificial intelligence
Finding more people with TB requires high-volume screening at both health care facilities and community mobile health screening events. Now, chest X-ray screening in both settings is aided by artificial intelligence (AI).
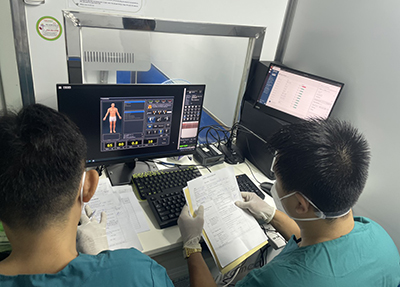
Radiologists interpret a chest X-ray and compare it with the artificial intelligence software’s interpretation. Photo credit: Phuong Nguyen/FHI 360
Using AI with chest X-ray helps ensure that people with TB are identified at all facilities, including lower levels of the health system where staff may have less experience interpreting chest X-rays. At community mobile health screening events, where one or two technicians may read hundreds of chest X-rays per day, AI helps avoid decision fatigue and over- or under-selection.
Since 2022, our project has used AI in community campaigns and high-volume district-level facilities to read more than 100,000 X-ray images. Ongoing AI data analysis is also informing targeted approaches for key and vulnerable populations. In addition, after several months, local radiologists and health workers reported multiple benefits:
“I read the chest X-ray first, without looking at the AI result,” says Dr. Mang Thi Thu Nhung. “Then, I look at the AI reading to compare the similarities and differences with my own reading. It helps me to improve when I see abnormalities the AI identified.”
“Sometimes we overlook small lesions or lesions covered by other organs. AI detects and marks these areas on the X-ray film screen,” says radiologist Ho Tuan Kiet.
Research has shown that automated AI interpretation of chest X-rays improves accuracy, but to date, there is no guidance on using it routinely within a TB program. The practical, data-informed implementation framework developed by our USAID Support to End TB team can help others plan and roll out AI as part of TB screening.
Accelerating TB case finding and preventive treatment

At a community TB testing event in Tien Giang province, Viet Nam, people wait to be tested in a mobile x-ray van. Photo credit: FHI 360 staff
The Double X strategy is one of the most accurate and comprehensive strategies for finding TB. In our project’s community campaigns, approximately 50% of people found to have TB had no symptoms and may have been missed without chest X-ray. In facilities, doctors say they’re now finding people with TB before they develop severe symptoms. When TB is found earlier, it’s easier to treat and prevents transmission.
Double X has become Viet Nam’s national TB screening strategy and continues to increase the use of advanced TB diagnostics. With backing from the Global Fund to Fight AIDS, Tuberculosis and Malaria and in collaboration with Viet Nam’s National TB Program, the project is providing Double X trainings nationwide.
Developing comprehensive, flexible TB strategies that address all stages of the disease is the way to end TB. We must continue updating practices and leveraging new technologies to detect, cure and prevent this ancient disease that continues to affect communities today.
